By David E. Stall, D.M.D.
Following the Patient’s First Year of Treatment
This case report follows a patient over their first year of treatment. The patient is a 69-year-old male who presented to our office. His chief complaint was that he had many broken teeth and wanted implants.
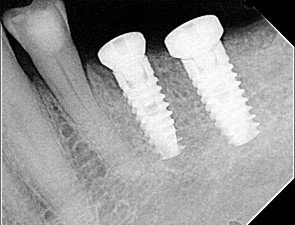
After a thorough dental and medical evaluation, including a complete set of x-rays and CBCT, a plan was developed for him. This included the removal of all broken and infected teeth, rebuilding the lower anterior teeth to improve his anterior occlusion, restoring the teeth that could be saved, and placing implants in the future edentulous sites of the lower arch. You can see on the x-rays and CBCT these areas.


Teeth #18, 19, and 20 were extracted during the first month’s appointment. The sockets were curetted of all granulation tissue, then corticocancellous bone and resorbable membranes were placed in #18 and #19, and an Osteogen bone/collagen plug was placed in the #20 site.
Teeth #29, 30, and 31 were extracted during the second month’s appointment. After all granulation tissue was removed, Osteogen plugs were placed in the #30 and 31 sites, but corticocancellous bone and a resorbable membrane were placed in the #29 site.
During the healing phase, treatment was rendered to the lower anterior and upper posterior teeth.
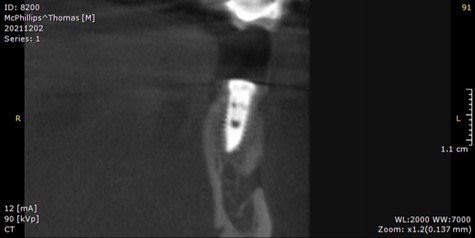
During the seventh-month appointment, a CBCT was taken to evaluate the bone-grafted site for implant placement.



At the eighth-month appointment, implants were placed in the #19, 20, 29, and 31 sites because the bone filled in nicely. Insertion torque was over 40 NCM for all implants. Healing screws were placed, and then we waited for osseointegration of the implants.
Two weeks after the eighth-month appointment, the patient presented to the office complaining of swelling in the buccal vestibule associated with implant #20. The patient was placed on Augmentin 500mg antibiotics for a week. The patient then returned for evaluation and treatment a week later.
It can be seen on the CBCT image that there is a loss of bone starting at the middle of the implant to the apex. The implant was not mobile, and a perio probe did not penetrate through the sulcus, indicating that bone was present around the occlusal half of the implant.
The patient was informed of the issue, and treatment began by creating a semilunar flap to expose the infected area.

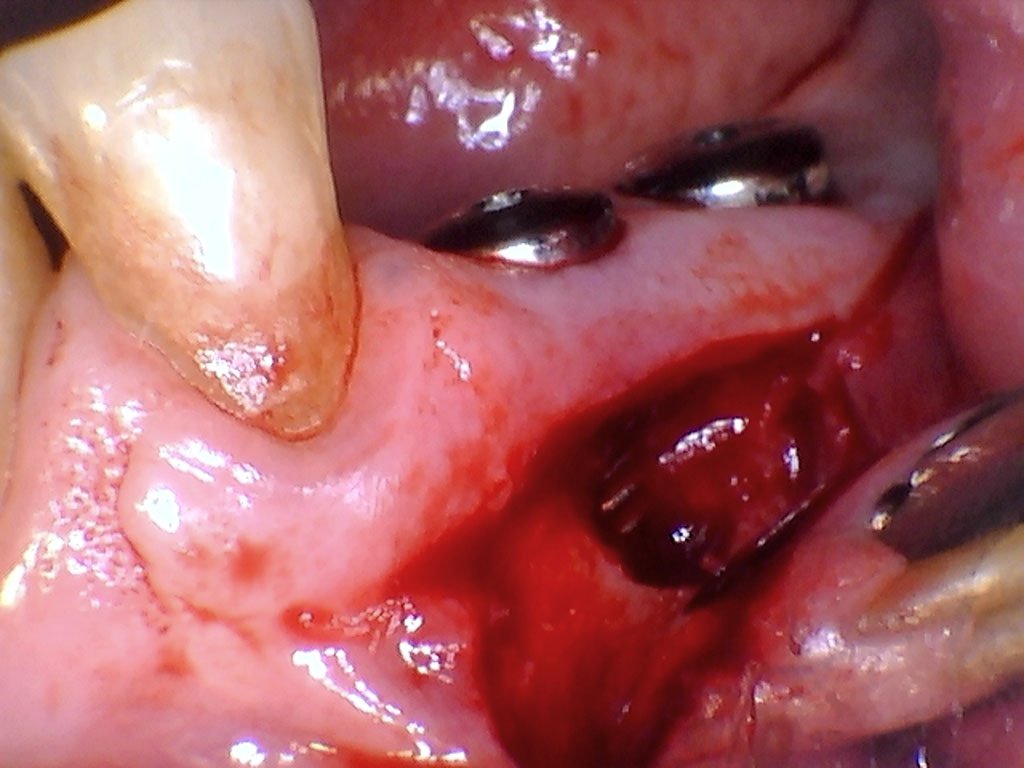
After curetting away as much granulation tissue as possible, the LightScalpel CO2 laser was used to vaporize the remaining infected tissue, sterilize the implant threads, and to de-epithelialize the margins of the flap. The laser was set at 4W, 20Hz, 2400mw, SuperPulse. The area was rinsed with saline, then corticocancellous bone, a resorbable membrane (Osteogen sheet) was placed, and the flap was sutured.
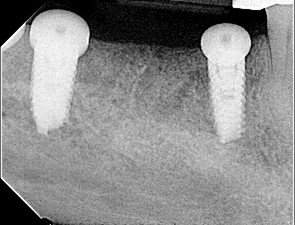
One-week and 3-week post-op checks showed no indication of swelling or infection, and the patient was comfortable.
In the twelfth-month appointment, another CBCT was taken to evaluate the bone over implant #20. It can be seen on the CBCT image that there was a significant improvement in the thickness of the bone.
Treatment to restore all the implants has begun, and the patient has had his lower teeth replaced.


LightScalpel CO2 Lasers and Periimplantitis
Unlike other common dental lasers, such as Nd:YAG and diode, LightScalpel 10,600 nm CO2 lasers can safely be used around dental implants without heating implant substructures. Compared to conventional peri-implantitis treatment, CO2 laser treatment results in more reestablished bone-to-implant contact.[1] LightScalpel CO2 lasers, unlike other dental CO2 lasers, use a flexible fiber delivery system making it easy to reach all areas of the mouth. Other benefits of the LightScalpel laser include minimized bleeding (which helps to maintain a clear surgical field), less swelling and discomfort for the patient, reduced risk of infection, shortened procedure times, and smoother recoveries. These clinical benefits make LightScalpel lasers an effective tool for treating peri-implantitis.
References
- Deppe H, Horch HH, Henke J, Donath K. Peri-implant care of ailing implants with the carbon dioxide laser. Int J Oral Maxillofac Implants. 2001;16:659-67.


